When Pregnancy Doesn’t Go “According to Plan”
you can still have a positive bith experience!
Samantha’s Birth Story
To fully tell my birth story, I have to start at the very beginning. When I found out I was pregnant with our first baby, I was so excited to have a dreamy, peaceful, water birth like all the videos I saw online. I thought if I did everything right, everything would go smoothly and I’d get the birth I always wanted (because that’s always how life works right?) Well, at my 21 week anatomy scan we found out we were having a baby girl. It was a Friday and we left our scan thinking everything was fine and excited to welcome our baby girl. Monday morning came and I received a call from my midwife, she wanted me to come into the office immediately, as they needed to talk with me. She was very vague and I tried not to let my mind wander to worry, what could be wrong with my perfect little girl that was kicking like crazy? My sister decided to come with me just in case it was something unexpected since my husband was over an hour away for work. The news I found out next rocked me to my core. Spina bifida. I had heard of it in my developmental biology class in college but it’s one of those things you never imagine could or would happen to you. I was young, healthy, taking all the right supplements (including folate), ate clean and exercised, and had absolutely no family history of any birth defects. How could this be? Spina bifida occurs in the first 28 days of pregnancy, often before a mother even knows she’s pregnant. When your baby is still just a ball of cells, folding and dividing, what is called the neural tube, later to become your baby’s brain and spine, folds into itself to form a tube (known as the neural tube). With spina bifida, the tube spontaneously does not close all the way at some point, almost like a zipper getting stuck part way, leaving a hole where the spinal cord is later exposed. Many doctors with outdated information would warn mothers “your baby will be a vegetables they’ll never walk, talk, know who you are” all of which couldn’t be further from the truth. Thankfully my midwives had all the latest information and assured me there were many closure options and the prognosis, while severe, was still good.
Many people with spina bifida go in to lead very normal lives with education, careers, families, it maybe just look a little different, as it’s very similar to a spinal cord injury. I was dumbfounded in complete denial I didn’t even know what questions to ask. My amazing midwives jumped into action and scheduled my MFM (high risk OB) appointments to get more info and there was talk that fetal surgery might be an option but I was so overwhelmed I didn’t know where to start. The tears flowed freely that first week but action quickly replaced dread and we were ready to see what could be done for our little girl. Before I knew it I was flying across the country to Johns Hopkins to meet with their Fetal Therapy team to discuss fetoscopic surgery as an option to close our daughter’s spine in utero.
While most babies with spina bifida have their spines closed at birth, there was a newer option to have surgery while still in the womb, where they delicately and carefully close your baby’s spine and place them back in to keep baking as long as possible. Fetoscopic surgery takes that a step further doing the procedure laparoscopically with two tiny ports, using pinchers and a camera, even less risk for me and baby. My head was swimming with all the new terms, understanding the huge amount of risk that came with the surgery (prematurity, early labor, even death for me or her). All I knew was that the benefits it could provide her seemed to heavily outweigh the risks in our circumstances and I was a perfect candidate for the surgery. Things moved incredibly fast and within 2 weeks of finding out about her diagnosis, at just 24 weeks pregnant, I was on the operating table. I’ll spare all the intense details, but recovery was brutal. It was the most painful thing I ever endured, I could barely get out of bed the first 3 weeks. My husband and my parents took turns taking care of me round the clock. It was intense trying to heal and keep my baby in. But after 3 weeks I was finally turning a corner. I felt less pain and more alert, the days blended together on bedrest but I was extremely grateful to be able to stay at the Believe in Tomorrow children’s house (very similar to a Ronald McDonald house) right across the street from the hospital. I made friends with other parents and families dealing with all different kinds of diagnoses for their children and while I felt like I was in “baby jail” I was optimistic. At my 3 week follow up appointment I found out I had global membrane separation, where my amniotic sac had come away from uterus wall due to the surgery. I was concerned but baby girl was still doing amazing, we were keeping my contractions from a very irritated uterus at bay and things seemed otherwise okay.
Another 3 weeks passed by to the day and I woke up to use the bathroom one morning to find my mucous plus and some fluid plopped right on out. My dad was on duty that day and he rushed me over to labor and delivery. They started an immediate magnesium drip (which in all honestly felt like it was going to kill me) and thankfully we held off labor. They admitted me to their antepartum unit and I spent another whopping 3 weeks of days blended together in the hospital. I learned a lot in my time there, I advocated for myself, said yes and no to policies, procedures, and medications I was okay and not okay with, had a great relationship with my nurses, requested the few I didn’t like to not be placed with me again, and ate a lot of moral support in Justin’s peanut butter cups. It was extremely lonely but my faith heavily carried me through with the strength of the Lord. I repeatedly lost my mucous plug and fluid and could tell labor was imminent, but thankfully my daughter handled it perfectly. The contractions were getting stronger and more frequent, although still random and varied. I was still hoping for a vaginal birth and my daughter was still head down until about 2 days before I went into labor. Suddenly the frequent ultrasounds showed she had flipped firmly butt-down and wasn’t budging. I knew labor was close, I felt like a distressed animal cooped up in the hospital room. I slowly walked the halls to pass the time and nested what little I could in my room tidying up and moving things around. I felt restless and my body and instincts knew the end was close.
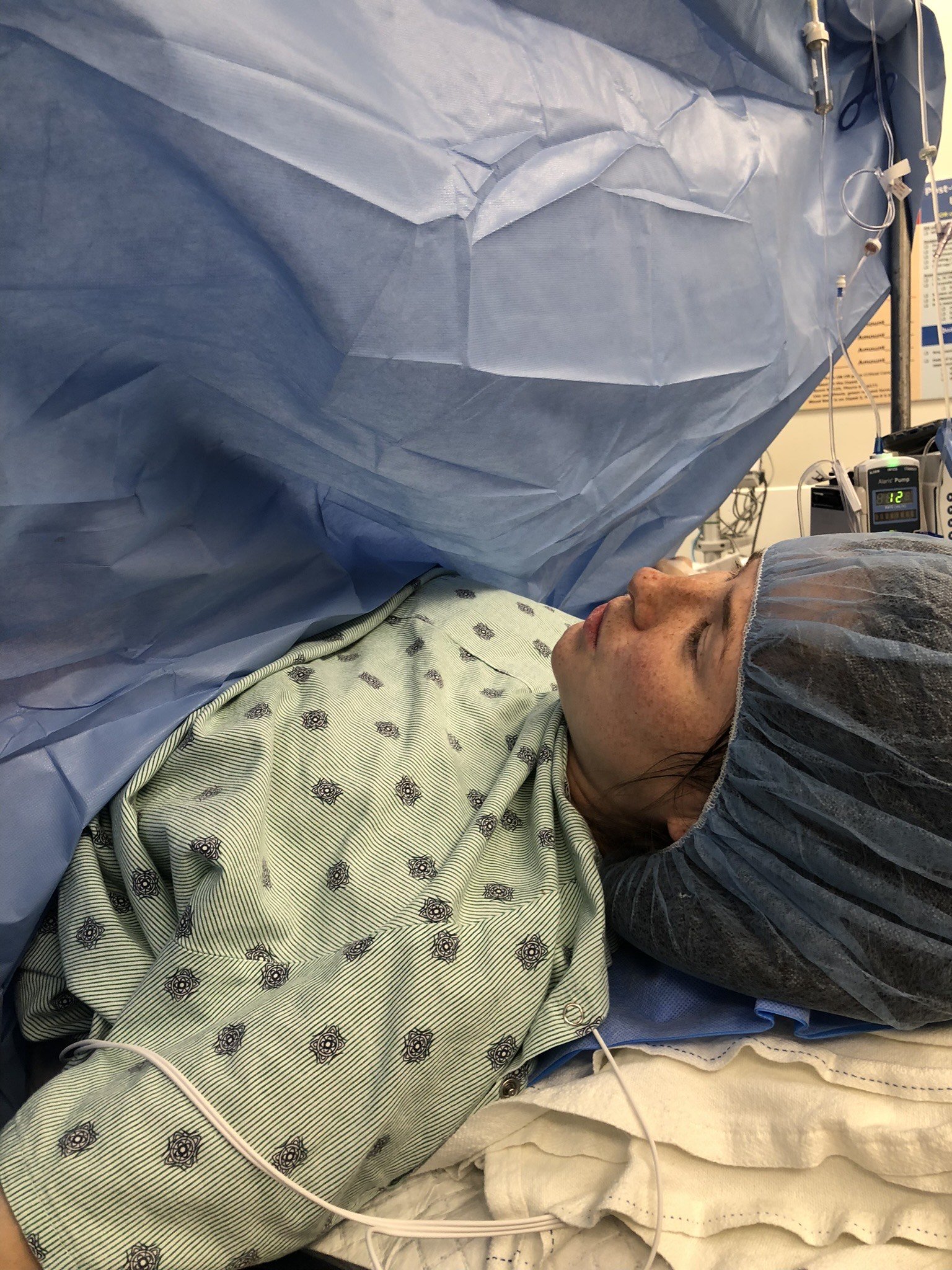
Some trouble with an IV they insisted I have the whole time led to my stress levels increasing on a Friday evening. By Saturday night I noticed my contractions had become regular 3-5 mins apart and STRONG. Suddenly I was having to breathe through them and focus and the pressure on my cervix changed, it felt sore and much different. I texted my in laws that I thought I might be in labor and that it might be baby time, as my parents were sick with the Flu. My MIL knew immediately this baby was coming and jumped in the car. They checked my cervix not long after and I was not surprised one bit to hear that I was dilated about 2 centimeters! Out of everything that was out of my control, I was ecstatic to feel what real labor contractions felt! I fully embraced breathing into them and relaxing as they prepped me for my inevitable c-section. I used all my labor prep knowledge I had accumulated over the years and was so grateful to feel my body doing something naturally for once. My nurses were incredibly kind and thankfully my favorite MFM OB who helped preform my fetal surgery was on call to do my csection. I felt strangely at peace and slightly relieved that it was all coming to an end after 9 painful and stressful weeks after the fetal surgery. I was so ready to meet my baby girl and was exhausted. My mother in law and sister in law made it with minutes to spare as I was being wheeled back into the OR. I’m very lucky to have a wonderful relationship with my MIL, who had also had a C-section before and knew exactly what to do. She help my hand and talked me through it and took a bunch of pictures. They’re still hard to look at but I’m grateful for them.
They placed my spinal block on the operating room table while the OR crew swirled around me like a pit crew. They let me pick a playlist to play for the surgery and I’m so grateful I had some familiar country music to listen to that helped me relax. I breathed through the tugging, which was more aggressive than I anticipated, and tuned out the voices. I did my best to breathe through it all and some waves of nausea came and went. I even felt faint at one point. Normally I have an iron stomach and genuine curiosity for all things medical but quickly learned I don’t feel the same way being the patient. In less than 10 minutes my baby girl was born at 12:08 am. It took her a minute to cry, the longest minute of my life but suddenly the tiniest, high-pitched cry I’ve ever heard erupted into the room and everyone breathed a sigh of relief. At 32 weeks and 5 days, my beautiful baby girl was born, 7 weeks early but otherwise totally healthy, her spine totally closed, and everything we had hoped for with the surgery seemed to have worked.
They honored my request to wait a few minutes to cut her cord, something I was so grateful for to have honored even with all the rest of my options being taken away. They proudly held her up for me to see with a little hat and blanket wrapped around her with a lining of plastic wrap against her tiny 3lb 10oz body to keep her tiny body warm. My MIL snapped a few pictures, and just like that my sweet girl was whisked away to the NICU to make sure she was stabilized and breathing properly. It would be another 8 hours before I saw my baby again. No skin to skin. No golden hour. No nursing. No bonding. Nothing I had hoped and dreamed for.
Unfortunately, as well as my daughter did those first few hours, my experience was less than positive. In the C-section they lost my IV due to their policy to always have an IV placed while I was inpatient. This ended up blowing out all the veins in my lower arms leaving virtually no options by the time I actually needed an IV for my C-section. The resident anesthesiologist was less than pleasant and hit a nerve while trying to place a new IV and was rude to me when I shouted at him that it was hurting me. Additionally there was a new resident OB helping with my C-section. At one point I heard her go “oops” mid surgery which prompted me to ask “is everything okay?” My OB quickly assured me that everything was fine, the resident just retracted too hard and ripped my incision open a little further. I’m not sure if her mistake had anything to do with this but we would find out two weeks later that I had sustained a rectors sheath hematoma and had lost over 2 units of blood bleeding internally from it.
However the surgery was over as quickly as it began and they brought me to recovery where I felt immediately requested a pump to start pumping in hopes that my milk would come in. I knew I wanted to desperately be able to breastfeed my daughter if I could help it. I was incredibly supported by all nurses and lactation consultants in that department which I was so grateful for. By the time I made it back to my hospital room I was exhausted and fell into a medicated slumber around 3 am. The next day once I had the strength I had my MIL wheel me over to the NICU where I was able to finally hold my daughter but something still didn’t feel right. I was extremely pale. I kept getting nerve pain in my shoulder that they assured me was just trapped gas from the C-section working its way out and I wrote it off. The only way I can describe what happened next was divine intervention.
The nerve pain became excruciating to the point where I was screaming for help. They rolled me down to a CT scan worried I was having a pulmonary embolism. Thankfully that was not the case but at the edge of the scan they spotted something unexpected. A massive blood clot in my leg. I had no symptoms, no pain, no swelling, nothing to indicate it was there. If my daughter hadn’t flipped breech, if I hadn’t had the C-section, if I hadn’t had the random nerve pain (we still have no idea what caused that), we never would have found the blood clot. We thankfully were able to totally dissolve it with blood thinners but I still am so thankful for the Lords faithfulness with orchestrating all of that. By then I was truly exhausted. Barely any sleep 24 hours later, barely seeing my daughter, pumping a massive amount of milk (my milk came in so strong I could have fed 3 babies), and the stress of a very scary medical finding I was tapped out. Thankfully my husband arrived from Montana the next morning and we had our daughter to focus on.
While it wasn’t the birth I had hoped for, there were still so many aspects I still felt I was able to advocate for even with a max-intervention C-section. Much of my hospital stay taught me I can still advocate for myself and my baby while admitted and that hospital policy is not law! Our daughter spent 30 very uneventful days in the NICU and came home breastfeeding and is absolutely thriving to this day. Thankfully everything we hoped the surgery would do for her has worked. I pray my next birth can be redemptive and healing after such a stressful experience but I know it will all happen exactly as it should. Sometimes the Lords plans are much greater than ours and I’m beyond thankful for modern medicine for helping me and my daughter when we needed it.